

David B. Hellmann,
MD, MACP
As I write this, the tulips outside my window are in full bloom and millions of people across the country and around the world are getting vaccinated against COVID-19. There’s a palpable feeling of hope in the air — hope for a post-pandemic future that promises relief from our long months of isolation, sacrifice and grief. And this issue of CIM Breakthrough reflects that spirit of hope.
I’m pleased to share, for example, that several of our faculty members are engaged in improving the quality of life of our rapidly aging population. For example, neurologist Alex Pantelyat, the Alafouzos Family CIM Human Aging Project Scholar, is tapping into the healing power of music to help patients with Parkinson’s disease improve their gait and speaking capacity — work that has now continued with community-based music programs. Cultivating community support for older adults is crucial for good health, as gerontologist Thomas Cudjoe — the Caryl and George Bernstein CIM Human Aging Project Scholar — has found, through his research and his house calls to aged patients. You’ll want to read about his efforts to combat social isolation (p. 8). And looking longer term, I’m exceedingly optimistic about the potential to dramatically reduce the negative health impacts of aging, thanks to the promising bench science of Qinchuan Wang, the Karen and Ethan Leder CIM Human Aging Project Scholar, who is collaborating with Mark Anderson, director of Medicine (p. 13).
Another cause for optimism: This spring, we inducted a new crop of exemplary doctors into our Miller Coulson Academy of Clinical Excellence (p. 16). And I was delighted to welcome Suzanne Koven to the (virtual) podium on May 4 to deliver the 18th Annual Miller Lecture. Dr. Koven spent her formative training years here at Hopkins, and now is the first writer-in-residence at Harvard’s Massachusetts General Hospital. Her new book, Letter to a Young Female Physician, offers hard-earned wisdom and insights that, I am confident, will help galvanize today’s trainees to become tomorrow’s great doctors.
Of course, the scourge of COVID-19 is not behind us yet, as Emily Brigham and Ann Parker can attest. They are among the co-directors of the Johns Hopkins Post-Acute COVID-19 Team (p. 2), a group committed to finding answers and treatments for the millions of COVID-19 “long-haulers” who continue to cope with debilitating health effects. The energy and expertise they bring to this daunting task is nothing short of extraordinary.
I am awed by all of these achievements and am most grateful to you, our generous supporters, for making this hope possible.

Aliki Perroti Professor of Medicine;
Vice Dean, Johns Hopkins Bayview Medical Center;
Chairman, Department of Medicine
Don Willett April 29th, 2021
Posted In:

David B. Hellmann,
MD, MACP
As I write this, the tulips outside my window are in full bloom and millions of people across the country and around the world are getting vaccinated against COVID-19. There’s a palpable feeling of hope in the air — hope for a post-pandemic future that promises relief from our long months of isolation, sacrifice and grief. And this issue of CIM Breakthrough reflects that spirit of hope.
I’m pleased to share, for example, that several of our faculty members are engaged in improving the quality of life of our rapidly aging population. For example, neurologist Alex Pantelyat, the Alafouzos Family CIM Human Aging Project Scholar, is tapping into the healing power of music to help patients with Parkinson’s disease improve their gait and speaking capacity — work that has now continued with community-based music programs. Cultivating community support for older adults is crucial for good health, as gerontologist Thomas Cudjoe — the Caryl and George Bernstein CIM Human Aging Project Scholar — has found, through his research and his house calls to aged patients. You’ll want to read about his efforts to combat social isolation (p. 8). And looking longer term, I’m exceedingly optimistic about the potential to dramatically reduce the negative health impacts of aging, thanks to the promising bench science of Qinchuan Wang, the Karen and Ethan Leder CIM Human Aging Project Scholar, who is collaborating with Mark Anderson, director of Medicine (p. 13).
Another cause for optimism: This spring, we inducted a new crop of exemplary doctors into our Miller Coulson Academy of Clinical Excellence (p. 16). And I was delighted to welcome Suzanne Koven to the (virtual) podium on May 4 to deliver the 18th Annual Miller Lecture. Dr. Koven spent her formative training years here at Hopkins, and now is the first writer-in-residence at Harvard’s Massachusetts General Hospital. Her new book, Letter to a Young Female Physician, offers hard-earned wisdom and insights that, I am confident, will help galvanize today’s trainees to become tomorrow’s great doctors.
Of course, the scourge of COVID-19 is not behind us yet, as Emily Brigham and Ann Parker can attest. They are among the co-directors of the Johns Hopkins Post-Acute COVID-19 Team (p. 2), a group committed to finding answers and treatments for the millions of COVID-19 “long-haulers” who continue to cope with debilitating health effects. The energy and expertise they bring to this daunting task is nothing short of extraordinary.
I am awed by all of these achievements and am most grateful to you, our generous supporters, for making this hope possible.

Aliki Perroti Professor of Medicine;
Vice Dean, Johns Hopkins Bayview Medical Center;
Chairman, Department of Medicine
Don Willett April 29th, 2021
Posted In:
 “It’s heartbreaking.”
“It’s heartbreaking.”
That’s how Johns Hopkins pulmonologist Emily Brigham describes her consultations with patients who continue to struggle with debilitating symptoms from COVID-19, months after their initial infection.
“Many of them had only minor COVID-19 symptoms to start, and here they are months later saying, ‘I can’t return to work. I can’t take care of my kids.’ They struggle with symptoms like intense fatigue, shortness of breath, heart palpitations and cognitive impairment. Tied to that are anxiety and depression. They are understandably very frustrated,” Brigham says.
Fortunately for these COVID-19 “long-haulers,” as they have come to be known, Brigham and fellow pulmonologist Ann Parker can connect them to a broad array of specialists to help support their recovery through JH PACT (Johns Hopkins Post-Acute COVID-19 Team), a service that both doctors launched and now co-direct with Physical Medicine and Rehabilitation colleagues, Alba Azola and Soo Kim.
Once patients’ specific needs have been identified and a treatment plan started, some receive care at home, including rehabilitation therapy and nursing visits. Others come to Johns Hopkins for services like physical, occupational and speech therapy.
“As early as March 2020, we recognized that because patients would have complex, multifactorial health needs, we would need to take a multidisciplinary approach.” – Ann Parker
Rehabilitation psychology, neuropsychology and psychiatry also provide key services to address patients’ cognitive and mental health needs. JH PACT also offers medication management in coordination with Johns Hopkins pharmacists, and COVID-19-related radiological imaging.
The idea for JH PACT came early on in the pandemic. “From decades of experience and research involving post-intensive care syndrome (PICS) — a collection of impairments in physical function, mental health and cognition that can persist for months or years after an ICU patient leaves the hospital — we expected there would be patients with COVID-19 who would be at risk for similar impairments,” says Parker. “As early as March 2020, we recognized that because patients would have complex, multifactorial health needs, we would need to take a multidisciplinary approach.”
Working closely comes easy for Brigham and Parker, who are good friends. They completed their Johns Hopkins fellowship training together and both bring important expertise to JH PACT.
JH PACT came together quickly, Brigham and Parker say, thanks to “amazing collaboration and support” from doctors, nurses and therapists from across Johns Hopkins.
Brigham is an expert in airway diseases like asthma and COPD, and she has done research examining disparate health outcomes among minority populations in an effort to improve health care equality. She also has treated patients with lingering respiratory symptoms post viral illness, and so the respiratory complications that accompany post-acute COVID-19 are not new to her. Parker’s research has focused on improving health outcomes for survivors of critical illness coming out of the ICU. In that role, she is well familiar with PICS and has developed strong working relationships with colleagues in Physical Medicine and Rehabilitation at Hopkins — specialists who are key to providing care for those with post-acute COVID-19.
“We sat down together in March, with pulmonologist Sarath Raju and Christian Merlo [pulmonary director of outpatient clinical operations], and said, ‘We need a service. Let’s hit the ground running with streamlined care for patients who will inevitably be coming to us post COVID-19,’” recalls Brigham. JH PACT came together quickly, Brigham and Parker say, thanks to “amazing collaboration and support” from doctors, nurses and therapists from across Johns Hopkins, including trainees like Jacqueline O’Toole and Sandra Zaeh (senior Pulmonary fellows).
In the midst of it all, Parker gave birth to her third son in May. “From March until he was born, I shifted from working directly with patients in the ICU. Instead, I was able to put systems in place to get JH PACT up and started,” she says.
“Ours was one of the first post-COVID-19 services in the nation and we were very proud we were able to do this. It really speaks to the breadth and depth of expertise here at Johns Hopkins.” – Emily Brigham
“Ours was one of the first post-COVID-19 services in the nation and we were very proud we were able to do this. It really speaks to the breadth and depth of expertise here at Johns Hopkins,” says Brigham.
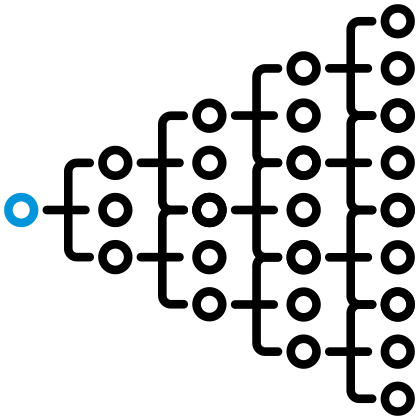
Because COVID-19 long-haulers come in with such a variety of different symptoms, involving all of the body’s major organ systems, she says, it’s critical to have access to an array of subspecialists: cardiologists, nephrologists, infectious disease specialists, hematologists, psychiatrists and more.
“With JH PACT, when I see a patient with all of these different systems, I can connect them to the appropriate care in a way that is relatively fast,” says Brigham. “And because our specialists are seeing many individuals with similar concerns, they are starting to see patterns, and they feedback to us.”
That feedback is an important element of JH PACT, notes Parker. “From the very beginning, we have been completing our clinical assessments in a very deliberate and standardized way, so that we can begin to recognize patterns and compare outcomes — across Johns Hopkins, the United States and internationally — with the ultimate goal of improving care for patients with post-acute sequelae of COVID-19 (PASC).”
Toward that end, there are efforts well-underway to launch a Johns Hopkins-wide data registry that will hold health information from the electronic medical records of patients who have been treated for COVID-19. The registry will offer a treasure trove of data that Johns Hopkins researchers can tap as they investigate new protocols and treatments for COVID-19 and post-acute COVID-19. There are also plans to establish a biorepository, with samples of body fluids and tissue from patients with COVID-19. Brigham and Parker believe such a biobank will prove crucial for future research efforts. “Having the availability of specimens will allow us to recognize patterns, ask questions, and rapidly answer those questions,” says Brigham.
These efforts have taken on increased urgency as evidence shows that a notable percentage of COVID-19 survivors (some estimate as high as one-third) continue to be plagued with life-altering symptoms long after they recover from acute illness.
“Sitting down with these patients, seeing their pain and frustration, and not being able to tell them when their symptoms will go away…it only drives us to come up with strategies as quickly as possible,” says Brigham.
Don Willett April 29th, 2021
Posted In:
 While the stay-at-home orders brought by COVID-19 led to countless canceled events and an end to in-person meetings, there has been one silver lining for members of CIM’s International Advisory Board and other CIM affiliates.
While the stay-at-home orders brought by COVID-19 led to countless canceled events and an end to in-person meetings, there has been one silver lining for members of CIM’s International Advisory Board and other CIM affiliates.
“Our CIM seminars, which used to be held in my office and attract at most 25 or 30 participants, moved to a Zoom format and our attendance has skyrocketed,” says CIM Director David Hellmann. “We routinely draw 50 or 75 people, and attendance at one seminar about COVID-19 surpassed 170 participants.”
Among those is board member Susan Immelt, a retired nurse, who says she has blocked out Tuesday afternoons at 4 p.m. on her calendar in anticipation of the Zoom seminars, which are scheduled about twice a month. “In this past year with so little structure, the CIM seminars have been a very welcome event to look forward to. They are phenomenally well done,” says Immelt, who together with her husband funds pulmonologist Brian Garibaldi as the Douglas Carroll, MD, CIM Scholar, in honor of her father.
The format of the seminars is straightforward. At each session, a keynote researcher whose Johns Hopkins work is supported by the Center for Innovative Medicine takes 30 to 40 minutes to share the scope and progress of that work in an accessible way, which some liken to a TED Talk. Subjects range widely: from the latest advances in detection of pancreatic cancer, to housing policy and health equity, to the importance of addressing isolation in the nation’s aging population. Then the floor is open for questions, and a lively back-and-forth ensues.
“I’ve been in a self-imposed lockdown here at my home in Danville, Kentucky, and when the CIM seminars moved to Zoom, I was just elated,” says board member Dana Case, also a retired nurse. “The presentations really expand my knowledge base and it makes my heart sing to see Johns Hopkins and the Center for Innovative Medicine doing so much good to benefit the world.”
Case adds, “As I learn new things I pass them along, and I’ve found the seminars to be a great way to connect with others.” For example, she invited her granddaughter, Kennedy, a law student in Rhode Island, to attend several meetings. “It’s given us a lot to discuss and she has taken information we learned during a seminar about COVID-19 to her legal internship in Nashville. She designed a database to help employees throughout the United States discern when they would be eligible to receive a COVID-19 vaccination.”
The seminars have also provided an outlet for Case to connect with her sister, fellow CIM International Advisory Board member Mary Ousley, also a registered nurse. (Both were integral to the inclusion of nurses in CIM’s Good Doctor Initiative, which is part of the Aliki Project.) “We usually text back and forth during the meetings or call once the session is over to talk through the material in more detail,” says Case. “It really elevates my thinking.”
Immelt concurs. “Most of the talks hit me right at the edge of my knowledge base — I know enough to understand what they’re covering but I am also learning something new.”
“The presentations really expand my knowledge base and it makes my heart sing to see Johns Hopkins and the Center for Innovative Medicine doing so much good to benefit the world.” – Dana Case
CIM International Advisory Board member Mark Rubenstein, who earned both his B.S. and M.S. from the engineering school at Johns Hopkins, says he was particularly struck by a presentation about the new Engineering Aging Alliance, which is part of Hopkins’ Human Aging Project, an initiative launched and supported by the CIM.
“I’m an engineer, so I was very interested to learn about what they’ve got planned,” says Rubenstein. The Aging Alliance is bringing together teams of clinicians, trainees and students — in engineering, medicine, nursing and business — in “innovation incubators” to come up with technological solutions to promote healthy aging.
Though he’s been officially retired from his career in commercial real estate now for 18 years, Rubenstein has remained very busy with a full schedule of daily business meetings, even during the pandemic. “Fortunately, however, my late afternoons on Tuesday are free, so I log on to the CIM seminars whenever I can,” he says. “There’s just so much great information.”
Don Willett April 29th, 2021
Posted In:
 For Hopkins geriatrician Thomas Cudjoe, making house calls to older patients throughout Baltimore City is a critical part of his day’s work, thanks to the Johns Hopkins Home-Based Medicine (JHOME) program, which provide in-home primary care services to individuals who are homebound and aren’t able to get to the doctor’s office due to medical conditions or physical problems.
For Hopkins geriatrician Thomas Cudjoe, making house calls to older patients throughout Baltimore City is a critical part of his day’s work, thanks to the Johns Hopkins Home-Based Medicine (JHOME) program, which provide in-home primary care services to individuals who are homebound and aren’t able to get to the doctor’s office due to medical conditions or physical problems.
“Home-based care is a great investment that our institution has made, and out of this experience I have seen firsthand the toll that social isolation has on older patients, particularly those with complex health needs who live in subsidized housing,” says Cudjoe, the Caryl and George Bernstein CIM Human Aging Project Scholar. “That’s why I’ve dedicated my professional life to understanding social isolation as an important health issue — and working toward solutions.”
Even before the COVID-19 pandemic, social isolation was a significant issue, impacting one in four older adults in the United States. And more than 40 percent of older adults reported experiencing loneliness. The impact on health is sobering, particularly among the homebound who are frail, depressed or cognitively impaired, Cudjoe notes.
“We know from multiple studies that social isolation is associated with higher levels of mortality,” he says.
“We know from multiple studies that social isolation is associated with higher levels of mortality.” – Thomas Cudjoe
In one avenue of his research, Cudjoe is looking to advance the science of social isolation, or as he puts it, “the way that social isolation ‘gets under our skin’ through biological pathways.” In early work that he presented recently at the Gerontological Society of America Meeting, which drew on data from the National Health and Aging Trend Study, he reported an association between social isolation and two key biomarkers for inflammation.
“These findings are important,” Cudjoe says, “because they indicate that social isolation is an important factor that has biological influences…which may potentially lead to poor health outcomes.”
Given the health implications for older adults, says Cudjoe, it’s important for geriatricians and other primary care providers who treat older patients to routinely assess social connectedness. Questions like “Do you feel left out?” or “How many people do you feel you can depend on or feel close to?” should become a routine part of each health visit, he believes, in much the same way that geriatricians regularly monitor blood pressure and weight. “On a public policy level,” he says, “advancing regular assessments for social connectedness is critically important.”
Once social isolation has been identified, what strategies can be employed to help connect older adults who are and feel isolated?
Leveraging technology is one possible solution, Cudjoe notes. During COVID-19, the almost overnight switch to telemedicine — prompted by shelter-at-home orders — showed that smartphones and video-enabled technologies could be effective platforms for offering counseling and for connecting older adults to family and friends through virtual interactions.
But access to technology remains an important barrier, particularly among older adults of limited income or who are Black and Latino — populations particularly hard hit by COVID-19 — as well as those struggling with vision or hearing loss or cognitive decline.
To reach a broader swath of the homebound, Cudjoe sees an opportunity to “harness volunteerism” and provide more support for organizations (such as Meals on Wheels) to provide regular in-person check-ins with older adults in the community. He points as an example to the “Call & Check Visits” in Jersey, British Channel Islands, where postal workers monitor and support older adults on their delivery routes with a knock on the door and a hello. Closer to home, programs like the AARP’s “Connect2Affect” provide a way to connect people with programs and technologies to increase their engagement.
“When thinking about solutions, it’s also important to remember that there are two sides of the coin and to acknowledge that there is heterogeneity among older adults,” says Cudjoe.
“Just as some older adults are isolated, there are others who are resilient and well integrated within their communities and contributing in so many different ways. What can we learn from those who are thriving?”
Don Willett April 29th, 2021
Posted In: